More Drug Users Are Intentionally Using Fentanyl Amid Overdose Crisis, Study Finds
Credit to Author: Luke Ottenhof| Date: Fri, 24 May 2019 18:00:26 +0000
Fentanyl has become shorthand in North American public discourse to indicate a dangerous, unwanted, and lethal substance. This is due to the opioid’s link to overdose crises across the continent. Opioid-related overdoses killed almost 4,000 Canadians in 2017, spurring policy advocates to call for legal, controlled drug supplies to help prevent more deaths. Provisional numbers from America’s Centers for Disease Control and Prevention attribute 30,000 overdose deaths across the country to fentanyl and related drugs. Since 2016, roughly 10,000 Canadians have died from opioid-related overdoses.
But while it’s widely understood that the powerful opioid as one that is contaminating drug supplies, new research suggests that this view is far too narrow, and could be impeding meaningful policy debate about how to deal with the opioid crisis.
A recent survey conducted by the British Columbia Centre for Disease Control (BCCDC) found that an increasingly large number of drug users are knowingly using fentanyl, a fact that might refocus public understandings of the opioid and open a conversation on the importance of access to safe drug supplies. Since 2016, roughly 10,000 Canadians have died from opioid-related overdoses.
The new study, carried out in 2018 and building on data from a 2015 survey, asked 486 users from 22 communities in British Columbia what drugs they had taken in the previous three days, running their answers against the results of lab-conducted urinalysis. Previous BCCDC studies used fentanyl test strips to identify the opioid, but the most recent study’s urine screen allowed researchers to detect a more comprehensive range of drugs present. Results indicated significant discrepancies between what users believed they had taken and what they had actually taken.
Among the study’s most important findings were statistics around fentanyl use. The opioid was detected in 92 percent of participants; of those participants, 64 percent were aware that they had taken fentanyl. This represents a drastic increase over information gathered during BCCDC’s 2015 study, which detected fentanyl in just 61 percent of participants. That same study reported that 73 percent of those individuals were unaware that they had taken fentanyl, while the new research puts that group at 36 percent. In the three years between the studies, reported use of fentanyl tripled from 13 percent to 39 percent.
“Previously, the discourse has been about [how] people using illegal opioids were unknowingly using substances contaminated by fentanyl,” Jane Buxton, medical lead for harm reduction with the BCCDC, said. “Our study suggests the majority of people who are using fentanyl know they are doing so.”
Buxton, who is also a professor and director with the University of British Columbia’s School of Population and Public Health, presented the results of the survey last month at Harm Reduction International Conference in Porto, Portugal. Buxton said that for this study, she and her colleagues purposely under-surveyed Vancouver to allow them to better understand drug usage in rural and semi-urban regions of BC. While most news coverage focuses on British Columbia’s urban centers, Buxton emphasizes that overdoses are occurring across the province.
Buxton explains that there are a number of possible reasons for the increase in knowing use of the potentially-lethal opioid. Individuals with substance use disorders might use opioids to manage pain and withdrawal symptoms, and if they can’t legally access prescriptions for pain-management drugs, they’re left to acquire opioids illegally. But as opposed to legal medical sources, these supplies aren’t safely and strictly regulated, meaning individuals accessing illegal opioids are vulnerable to danger.
“Despite people being aware they’re taking drugs containing fentanyl,” Buxton said, “they may have no alternative or access to a safer supply of known opioid content.”
The BCCDC’s findings indicate the severity and depth of the problem: fentanyl use is increasing even as the majority of overdose deaths are linked to the drug (in 2018, fentanyl was present in 87 percent of illicit overdose deaths in British Columbia). Buxton links this dire situation to “policies of criminalization [and] prohibition” which continuously fail to address overdose rates while tacitly bolstering unregulated drug supplies.
Buxton points to “a lack of understanding” as a major impediment in developing effective drug policy. “With an addiction [or] substance use disorder, just stopping or not using is not an option,” she said. “Some use to manage pain when a prescription is cut off, some to treat their withdrawal symptoms and be able to function.
“Lack of understanding and trying to ignore the issue, and ‘othering’ of people who use drugs, lead to stigma and support of abstinence-based policies, which for many don’t work.”
Canada’s recent legalization of cannabis—as well as an uptick in interest in legalization of all drugs—has drug users, activists, and researchers advocating for a future with fully legal and quality-controlled supplies. Buxton said that the need for a “safer, regulated drug supply” is a critical piece of policy among many that might help halt international overdose crises. She says this should include low-to-no-barrier access to opioid agonist therapy (OAT), which transitions opioid users to controlled long-acting opioids like methadone and suboxone which can help prevent cravings and withdrawal symptoms.
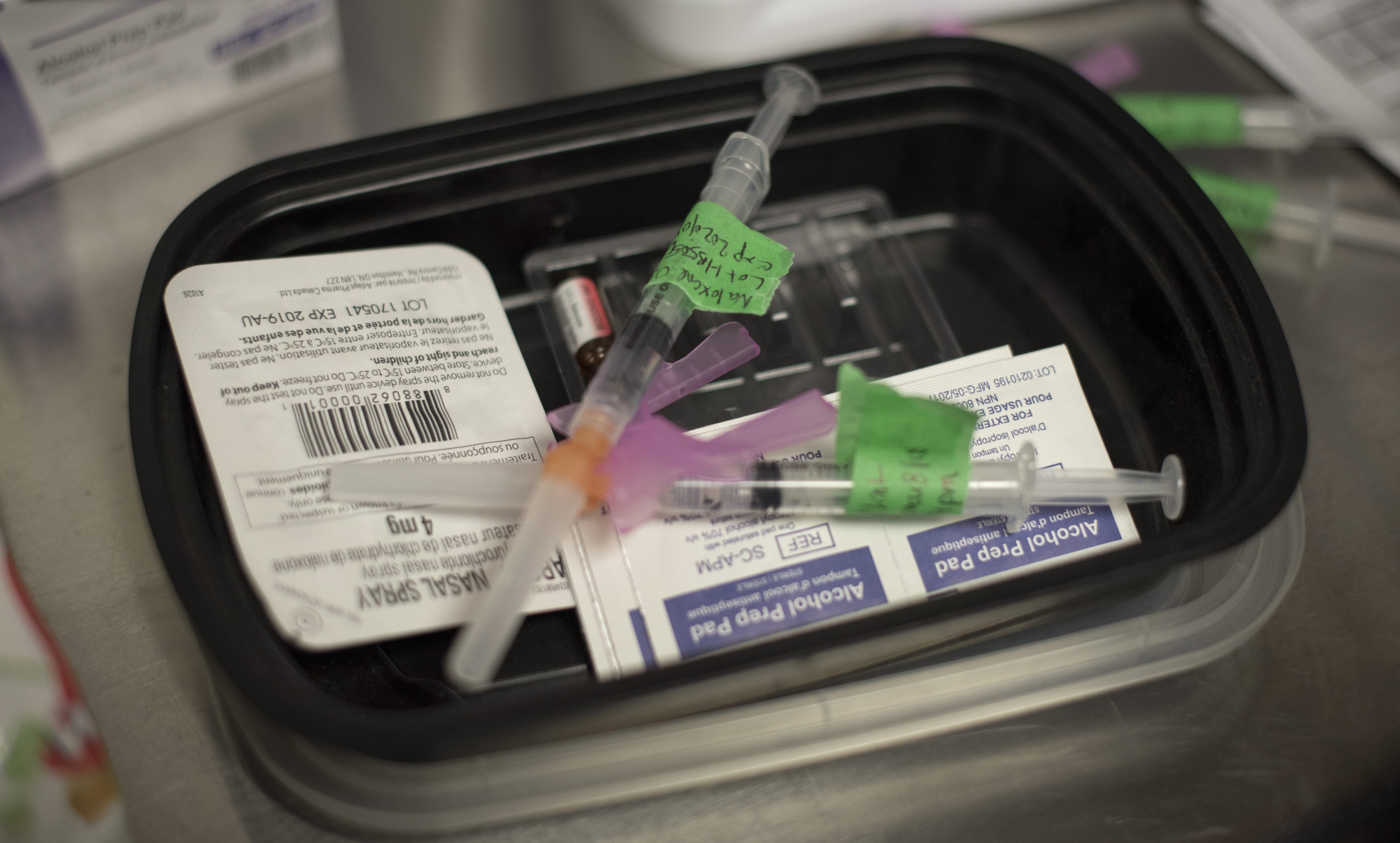
Buxton also points to other key supports, like expansion of take-home naloxone programs and an increase in safe consumption sites, as necessary parts of this plan. Over 144,000 naloxone kits have been distributed in British Columbia since 2012, with almost 40,000 reported overdose reversals—though some in Canada, like Windsor, Ontario police chief Al Frederick, are still fighting accessibility to the lifesaving kits. These take-home kits can be found at over 1500 sites across British Columbia. Check BCCDC’s site finder for information on where you can get one.
Follow Luke on Twitter.